Hepatic encephalopathy is brain damage caused by metabolic toxins. The cause is liver damage, most often liver cirrhosis. Decomposition products, especially ammonia, are no longer adequately disposed of. One of the consequences is hepatic encephalopathy.
What is hepatic encephalopathy?
According to AbbreviationFinder, hepatic encephalopathy is a crisis of the central nervous system resulting from liver damage. This leads to poisoning of the body due to the accumulation of metabolic products in the blood. The pathologically altered liver can no longer break down these “metabolites”. Especially the sensitive nerve cells of the brain suffer from the internal intoxication.
Doctors differentiate between 4 degrees of severity according to symptoms:
Grade 1: Reduced ability to concentrate and unstable mood
Grade 2: Extreme fatigue and slight disorientation
Grade 3: Somnolence, speech disorders, severe confusion, motor insecurity and incontinence (spontaneous loss of urine and stool)
Grade 4: unconsciousness and loss of reflexes and pain perception (hepatic coma: coma hepaticum)
root cause
In some textbooks, instead of this 4-stage classification, there is a differentiation of 5 degrees of hepatic encephalopathy. Hepatic encephalopathy is the result of serious liver disease, primarily advanced liver cirrhosis.
Causes are mostly chronic poisoning of the metabolic organ through excessive alcohol consumption in alcoholism. Intoxication with drugs or other chemicals can also be crucial. In addition, inflammation of the liver ( hepatitis ) or the bile and bile ducts are the reason for liver disease.
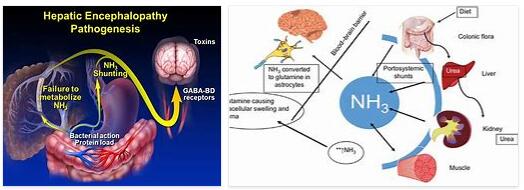
Under the stressful conditions, the liver cannot perform its detoxification function or can no longer adequately perform it. The lack of urea synthesis causes a build-up of ammonia in the bloodstream. There are also other bio-organic compounds such as nitrogenous acids and sulfur compounds. All of these metabolic products have a toxic effect on the brain in particular and lead to the formation of cerebral edema (water accumulation in the brain).
The result is an increase in intracranial pressure (brain pressure) with the result of mental impairments in the context of hepatic encephalopathy.
Symptoms, Ailments & Signs
Hepatic encephalopathy is characterized by variable neurological and psychiatric symptoms. In mild cases, there are often no symptoms at all. Or it is a slight reduction in general well-being. In the case of a fully developed hepatic encephalopathy, however, the so-called hepatic coma (coma hepaticum) occurs.
In terms of symptoms, the disease can be divided into four stages or degrees of severity. In stage I, mood swings, sleep disorders, sometimes euphoric states, slight confusion, tremors in the eyes and slight concentration problems occur. The symptoms can be so minor that they may not even be interpreted as a sign of illness.
In the second stage of hepatic encephalopathy, the symptoms become more noticeable. Among other things, personality changes, memory disorders, tiredness, disorientation, grimacing and severe trembling of the hands already occur here. The third stage of the disease is characterized by pronounced drowsiness, severe disorientation, tremors in the hands and unclear speech.
The patient sleeps all the time, but can still be awakened. In the fourth stage, however, the person concerned can no longer be awakened. This is no longer sleep but a comatose state. Symptoms intensify depending on the rate of liver failure.
In acute liver failure, stage IV of the disease is quickly reached. However, chronic liver disease often leads to chronic hepatic encephalopathy, which can alternate between severe and mild symptoms.
Diagnosis & History
Hepatic encephalopathy is initially nonspecific in its symptoms. However, the doctor quickly recognizes from the ammonia level in the blood that a hepatic crisis is present. Nevertheless, other diseases such as sugar shock in diabetes or a stroke must be ruled out at the same time.
The findings are substantiated by the usual liver diagnostics with liver values and sonography as well as computed tomography. An EEG reveals the patient’s tendency to have seizures. The classification into 4 stages also describes the possible development as the disease progresses.
Following acute forms, relapses can occur, while chronification often progresses to the end stage. The onset of death in complete liver failure is also due to hepatic encephalopathy.
Complications
Hepatic encephalopathy results from chronic liver disease. This disease can be harmless, but can also take a life-threatening course. The patient may initially appear drowsy and have trouble concentrating. In further stages, the person affected can fall asleep more and more with increased muscle tension.
This can go on until the person concerned falls into a life-threatening coma (coma hepaticum) with their own reflexes gone. Liver cirrhosis also has other complications. Thus, due to the hepatic remodeling of the liver, its performance of synthesis decreases. Fewer proteins are produced than are needed. This causes less oncotic pressure to build up in the blood.
Ultimately, this means that more water is squeezed out, leading to the development of edema. The coagulation proteins are also reduced, the patient has a longer bleeding time. It is not uncommon for a hepatorenal or hepatopulmonary syndrome to occur, which means that the kidneys or lungs can also fail over time.
In addition, the spleen usually enlarges, which causes pain in the upper left abdomen. Varicose veins can develop in the stomach area, which in the worst case can burst and lead to bleeding. The risk of developing liver cancer is also greatly increased in cirrhotic patients.
When should you go to the doctor?
A doctor should be contacted if the sufferer suffers from a disturbance of concentration over a long period of time. If the usual level of performance drops or if there is persistent listlessness, a doctor should be consulted. If the usual daily obligations can no longer be fulfilled, a doctor should be consulted.
If the person concerned obviously needs help because he can no longer cope with everyday life without care, a doctor must examine the patient’s state of health. Loss of muscle tone, changes in physical appearance, and disorientation are uncommon and should be investigated.
Caution should be exercised in the case of disorders of consciousness. If you lose consciousness, call an ambulance. To ensure that the patient does not die or have lifelong impairments, first aid measures must be provided until the emergency services arrive.
Confusion, tremors in the hands or body and inner restlessness should be examined and treated by a doctor as soon as possible. In the case of persistent tiredness, exhaustion, disturbances in attention or apathy, a doctor’s visit is also necessary. Involuntary muscle twitching, eye problems, unsteady gait and dizziness are reasons to consult a doctor.
Treatment & Therapy
Hepatic encephalopathy initially requires a reduction in the ammonia level. This is done by specifically influencing the intestinal flora, whereby the proportion of ammonia-producing bacteria is to be reduced.
In addition, the patient receives antibiotics, which act primarily in the intestines, since they are only slowly resorbed. Lactulose, an artificial type of sugar, promotes the growth of lactic acid bacteria, which means that the ammonia-forming substances take a back seat. A low-protein diet prevents excess nitrogen intake in the first place. For the patient, this means a purely vegetarian diet, which also contains no eggs or milk or any of their processed products.
The doctor achieves support of the liver function with drugs that promote the urea cycle, i.e. the elimination of nitrogen. The electrolyte balance ( minerals ) often has to be corrected, and at the same time the doctor has to prevent impending dehydration ( dehydration ). In addition, the administration of the trace element zinc is appropriate. In some cases, blood plasma purification must be carried out (therapeutic plasmapheresis).
Liver perfusion can be improved in some patients. Affected are people who have previously undergone surgical relief of the portal vein. If the blood pressure in the portal vein is surgically raised again slightly, the result is better supply to the liver. In the case of total liver failure, only a liver transplant can help as part of the overall situation with the complication of hepatic encephalopathy.
Outlook & Forecast
Hepatic encephalopathy can be cured with good and comprehensive medical care. This requires an early diagnosis and the fastest possible start of treatment. For some patients, symptomatic treatment is sufficient to achieve lasting relief.
Mood swings or liver dysfunction are alleviated by the administration of medication. The healing process of hepatic encephalopathy is generally described as reversible, provided there are no other disorders and treatment is sought.
The progression of the disease is progressive without medical and drug therapy, since no spontaneous healing is to be expected with this disease. The germs continue to spread in the organism and lead to a deterioration in general health and quality of life. In severe cases, the disease progresses despite treatment.
The permanently progressing process usually appears with episodic phases. With this clinically manifested hepatic encephalopathy, severe impairments in general lifestyle can be observed. In addition, the patient’s risk of death increases significantly.
The poor prognosis in these cases also depends on the underlying disease, the overall diagnosis and the start of treatment. However, the chronic course occurs only very rarely. In the event of acute liver failure, however, there is a risk of the patient dying prematurely.
Prevention
Preventing hepatic encephalopathy means protecting the liver with balanced eating and drinking habits. Alcohol and drug abuse as well as greasy food affect the central metabolic organ. Hepatitis infections can be prevented by general food hygiene. These measures serve to prevent liver diseases and ultimately also hepatic encephalopathy.
Aftercare
In most cases, those affected with this disease have no or only very few measures and options for direct aftercare available that can permanently alleviate the symptoms of the disease. In general, early diagnosis and treatment of the disease has a very positive effect on the further course and can also prevent other complications.
The priority with this disease is therefore early diagnosis, so that the person affected should consult a doctor as soon as the first symptoms and symptoms appear. In most cases, this disease is treated by taking antibiotics and other medications. The person concerned should always ensure that they are taken regularly and that the dosage is correct in order to permanently relieve the symptoms.
If anything is unclear or if you have any questions, you should always consult a doctor first to prevent further complications. Antibiotics should not be taken together with alcohol, otherwise their effect will be significantly reduced. In many cases, patients are also dependent on taking zinc, although this deficiency can also be controlled through diet. The doctor can create a nutrition plan for the person concerned.
You can do that yourself
Numerous factors precede the changes. The increased intake of proteins is one of the triggers. Likewise, dehydration and hypoxia. Dietary measures are beneficial in chronic hepatic encephalopathy.
Likewise, the intake of poorly absorbable antibiotics (e.g. Rifaximin) to reduce the ammonia – producing intestinal flora or the intestinal contents. The administration of lactulose is helpful for defecation. You can influence the reduction of the protein content yourself through your diet. Avoiding animal meat is also beneficial.
Hepatic encephalopathy is a sign of poor liver function that needs to be positively influenced. Alcohol and sedative medication should be avoided at all costs. The spectrum of changes ranges from mild symptoms to a coma hepaticus (hepatic coma).
In order to deal with the disease better, it is advisable to join a self-help group. The German Liver Aid, for example, is a non-profit association that was founded by patients 25 years ago. The German Liver Foundation also offers information material and supports patients, e.g. in the form of a hotline.